https://twitter.com/BlankName5000/status/1527586477118574593
Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threat
In March 2021, NTI partnered with the Munich Security Conference to
conduct a tabletop exercise on reducing high-consequence biological threats.
The exercise examined gaps in national and international biosecurity and
pandemic preparedness architectures—exploring opportunities to improve
prevention and response capabilities for high-consequence biological
events. This report summarizes the exercise scenario, key findings from
the discussion, and actionable recommendations for the international
community.
Published May 20, 2022
Is this a cover up for the covid vaccines?
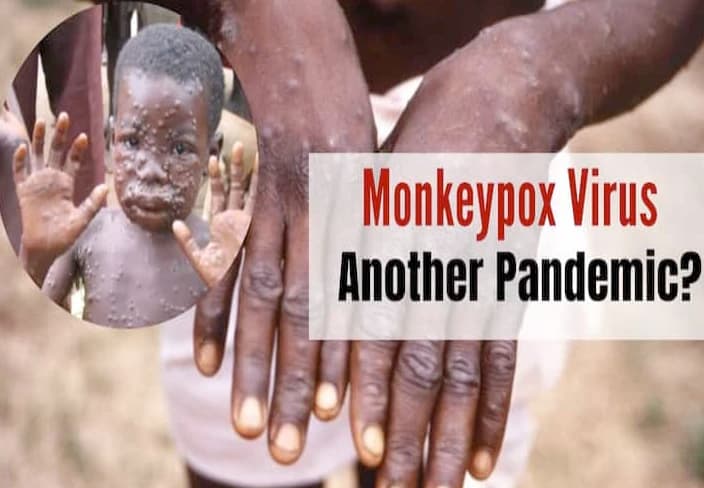
Rash, fever, chill, can be mistaken for chicken pox.
BOOM! The Public Health Mafia is caught red handed planning another 'outbreak' from which they can terrorize the public and make bank.
First half is a review of monkeypox over the years and the second half is the BOOM!
Emergence of Monkeypox as the Most Important Orthopoxvirus Infection in Humans
- Laboratory of Clinical Virology, Department of Microbiology & Immunology, Rega Institute for Medical Research, KU Leuven, Leuven, Belgium
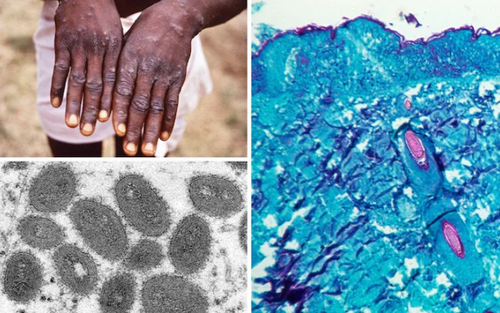
Monkeypox is an emerging zoonotic disease recognized as the most important orthopoxvirus infection in humans in the smallpox post-eradication era. The clinical presentation of monkeypox is similar to the one of smallpox. The case fatality rate of monkeypox (10%) lies between the case fatality rate of variola major (30%) and variola minor (1%). The disease is endemic in the Democratic Republic of the Congo, but other countries of Central and West Africa either reported cases of monkeypox in humans or circulation in wildlife. The disease was also imported once into the USA. The disease has always been considered rare and self-limiting, however recent sporadic reports suggest otherwise. Unfortunately, the collected data is limited, dispersed and often incomplete. Therefore, the objective of this review is to trace all reported human monkeypox outbreaks and relevant epidemiological information. The frequency and geographical spread of human monkeypox cases have increased in recent years, and there are huge gaps in our understanding of the disease's emergence, epidemiology, and ecology. The monkeypox virus is considered a high threat pathogen causing a disease of public health importance. Therefore, there is an urgent need to focus on building surveillance capacities which will provide valuable information for designing appropriate prevention, preparedness and response activities.
Introduction
Monkeypox (MPX) is an emerging zoonotic disease caused by monkeypox virus (MPXV), a member of the Orthopoxvirus genus in the Poxviridae family. MPXV is one of the four Orthopoxvirus species pathogenic for humans, together with variola virus, the causative agent of smallpox, now eradicated in nature; cowpox virus, and vaccinia virus (1). Monkeypox can infect a taxonomically wide range of mammalian species but the natural host is unknown. The virus has only been isolated twice from a wild animal, a rope squirrel in the Democratic Republic of Congo (DRC) (2) and a sooty mangabey in Ivory Coast (3). Transmission is believed to occur via saliva/respiratory excretions or contact with lesion exudate or crust material. Viral shedding via feces may represent another exposure source (4, 5). The clinical picture of monkeypox closely resembles the one of smallpox but the major difference distinguishing MPX from smallpox is the lymph node enlargement that occurs early, often at the onset of fever. A rash usually appears 1–3 days after the onset of fever and lymphadenopathy, with lesions appearing simultaneously, and evolving at a similar rate. Their distribution is mainly peripheral but can cover the whole body during a severe illness. The infection can last up to 4 weeks until the lesion desquamate (6). Patients can suffer from a range of complications including secondary bacterial infections, respiratory distress, bronchopneumonia, gastrointestinal involvement, dehydration, sepsis, encephalitis, and corneal infection with ensuing loss of vision. No specific treatment for a monkeypox virus infection currently exists, and patients are managed with supportive care and symptomatic treatment (7).
In an African setting, MPX can be misdiagnosed with other rash illnesses. The most common misdiagnosis [up to 50% of suspected MPX cases in the DRC (8, 9)] is chickenpox, also known as varicella, caused by varicella zoster virus (VZV). Coinfections with both MPXV and VZV were reported only a few times (8, 10, 11), however it was recently suggested that it is a relatively common phenomenon (12). The role of the VZV in MPXV epidemiology is not clear. Besides chickenpox, MPX can be misdiagnosed as cutaneous anthrax, fungal infection in HIV patients, Staphylococcus sp. related rash (13) or other diseases which cause rash.
Two genetic clades of Monkeypox virus have been characterized including the West African and the Central African clade. These two clades are geographically separated and have defined epidemiological and clinical differences. The West African clade demonstrates a case fatality rate (CFR) <1%, and no human-to-human transmission was ever documented. In comparison, the Congo Basin clade (also known as the Central African clade) show a CFR up to 11% (14), and documented human-to-human transmission up to 6 sequential events was observed. The isolates from the West African clade originated from outbreaks in Nigeria, Liberia, Ivory Coast, Sierra Leone, and USA (imported from Ghana) while the isolates belonging to the Central African clade came from Gabon, Cameroon, the Republic of Congo (ROC), Central African Republic (CAR), Sudan, and the DRC (14–17). According to available data, the Congo Basin clade is more common than the West African clade given it is endemic in the DRC where more than 2,000 suspected cases are reported every year (18). However, MPX is not part of mandatory reporting in other countries than the DRC, which might introduce a bias (19).
MPX has always been considered a rare sporadic disease with a limited capacity to spread between humans (20). Nonetheless, it is a life-threatening disease in the DRC and other countries of western and central Africa (8) and possibly worldwide. The threat would increase if there would be a virulence increase [both naturally (1, 21) or through genetic engineering (22)], a virus spill into more widely distributed taxa (23) or an introduction in other continents (24). Consequently, MPXV belongs to the “biosafety level 3” category, the “high threat” biodefence category in the EU (25) and is on the list of select agents in the USA (26).
The scientific community is hesitant to the importance of MPX which can be demonstrated by a limited number of research articles in the biomedical literature. The biggest number of articles was published in a year when MPX was reported outside of the African continent for the first time in history. In the past decades, we have seen a similar reluctance to research and control of other pathogens with epidemic potential (Zika and Ebola as recent examples) which were geographically limited to the Southern Hemisphere.
Monkeypox outbreaks are rarely reported, badly managed and little described leading to an incomplete picture of the disease's importance. MPX is the next most pathogenic poxvirus disease after smallpox but never received appropriate attention to prevent it to become an epidemic. The next sections attempt to summarize all publicly available literature on human monkeypox cases, both official and unofficial, since the first case in 1970 until 2018.
Outbreaks of Monkeypox in Humans
1970–1990
The first human MPX case was reported in August 1970 in Bokenda, a remote village in the Equatorial province of the DRC (called Zaire at the time). A 9 month old child was admitted to Basankusu Hospital with suspected smallpox (56) and a sample, sent to the WHO Smallpox Reference Centre (Moscow), revealed MPXV by virus isolation (57). The patient's family said that monkeys were eaten occasionally as a delicacy but they were not able to recall if monkeys had been eaten during the last month or if the child came into contact with a monkey lately. The investigation showed that the child was the only one in the family who had not been vaccinated against smallpox (56).
The first 20 human cases were described by the WHO (42, 58, 59) in 1972 and 1976, and 15 newly reported cases were included in the update of 1978 (60). Later, WHO reported 54 cases between 1970–1979 (20, 30, 61), out of which 47 were described by Breman et al. (43). JeŽek et al. reported 59 cases between 1970 and 1980 (27, 62). This number of 59 cases was also reported in one of the later reviews, but no reference was mentioned (28).
The Global Commission for the Certification of Smallpox Eradication designated MPX as the most important orthopoxvirus infection in men in the post-smallpox eradication era (from 1980). They recommended in their final report in 1980 that a surveillance program on MPXV and its epidemiology and ecology should be continued (63). After 1980, the number of reported cases among reports differ. Arita et al. reported 98 cases (61), a WHO meeting counted 100 cases (20) and JeŽek et al. reported 132 cases between 1981–1983 (62). Between 1980 and 1986, a total number of 350 (30) and 346 (62) cases were reported. The WHO active surveillance program between 1981 and 1986 identified 338 confirmed monkeypox cases and 33 deaths (CFR 9.8%). The increase in MPX cases between 1981 and 1986 was probably due to strengthened surveillance since there was no substantial increase in the number of cases coming from the areas not under the WHO surveillance (27).
Although the number of yearly reported cases in different countries varies among sources, the total number of confirmed MPX cases reported per country from 1970 till the end of 1986 is the same, resulting in 404 cases (30, 64). Some sources report 404 cases during the WHO surveillance period (1981–1986) alone, but without (6, 28) or with an incorrect reference (24).
Human-to-human transmission occurred occasionally from primary human cases but very rarely from secondary cases (61). There was no increase in the secondary attack rate for household contacts from the period 1970–1980 (12%) to the period 1981–1986 (9.28%) thus there was no evidence for a change in transmissibility of the virus (4). The longest reported chain of inter-human transmission consisted of four serial cases, which indicated little potential of the virus for epidemic spread (27, 65). Primary infections from animals were responsible for 72% while inter-human transmission accounted for 28% (29, 66). Children below 10 years of age accounted for the majority (86%) of cases (6, 27). Males (58%) predominated females (42%) among the primary cases (especially in the age group 5–14 years), while female patients were more common among the secondary patients. It showed that the unvaccinated young males were at greater risk for infection, probably because they trapped and played with small rodents and their carcasses. Females were at risk because of child-to-mother infections (27). Local population immunity from the smallpox vaccination was estimated at ≥60% during the 1970s and the early 1980s (29). Almost all primary cases occurred in unvaccinated individuals (average annual primary attack rate of 1.7 per 10,000, compared to a rate of 0.04 per 10,000 among those vaccinated) (27). Sera of 774 unvaccinated contacts of reported cases were taken during the WHO surveillance (1981–1986) and 136 (18%) of them had been infected with MPXV (27).
The number of reported cases dramatically decreased after the intensified surveillance was discontinued. Outbreaks were reported from Gabon in **1987 [**44] and the DRC (called Zaire at the time) between 1987 and 1992. However, the numbers of reported cases differ between sources and the year of the outbreak in the DRC is not clear (28, 29, 40, 48)....
Years inbetween included in article:
In 2014, a MPX outbreak was reported in Sierra Leone (Bo City) after more than 40 years. Only one case was lab confirmed (40, 47) and the total number of infected people is not known.
From December 2015 till February 2016, at least 12 people (out of which 3 died) got infected with MPXV in Bangassou, Mbomou province, the CAR. The disease was confirmed by the laboratory of the Ministry of Health (37, 72, 83). Journal de Bangui (72) stated in the report announcing this outbreak that there was recently a mokeypox outbreak 2014 in Haute Kotto zone. There is no further information to support this so the validity cannot be confirmed.
CAR (Basse-Kotto and Haute-Kotto provinces) experienced at least 26 more suspected cases (of which at least 3 were confirmed) as of August 2016 (38, 84).
Between September 2014 and February 2016, 587 suspected MPX cases were reported through a passive surveillance program of the DRC. The majority of reported cases were located in the Equateur province (363 cases) and the Tshuapa province (135 cases). The other provinces accounted each for 18 or less cases during this period. 55% of all suspected cases were male. 320 suspected cases were younger than 15 years, 256 were 15 or older. 592 clinical specimens were obtained from 339 patients which represents 57.8% of all reported suspected cases. 223 tested positive for MPXV, 40 for VZV and 78 for neither. There were two cases of coinfection with both, MPX and VZV (85).
Between January and August 2017, ROC, Likouala province reported monkeypox outbreak accounting for 88 cases out of which 7 were laboratory confirmed, including 6 deaths (CFR 6.8%). A total of 18 villages in 5 districts (Enyelle, Betou, Dongou, Impfondo, and Owando) have been affected (54). The outbreak was formally declared by the Congo state authority on 13th March. Children under 15 years of age were the most affected, accounting for 60% of the overall caseload. The gender distribution was proportionate, with 51% of the cases being female (86). This was the biggest outbreak of monkeypox reported in the ROC with high transmission potential probably due to prevalent underlying exposure risk factors in the communities. WHO considered the overall risk of this outbreak high at national level given the weak surveillance system coupled with the limited public health infrastructure. In addition, the risk of disease spreading to the neighboring countries was also considered high in view of the high population mobility and the presence of refugees from Central African Republic, Democratic Republic of Congo, and Chad (86). Monkeypox occurs in African countries which often have weak surveillance and public health infrastructure making the prevention and response difficult.
Two outbreaks were reported in CAR in 2017. The first outbreak was reported in Mbomou province in February 2017. Limited information is available for this event. 47 cases (5 confirmed) were reported by WHO in the bulletin of week 22 (87) however only 5 cases (2 confirmed) were reported in the bulletin of week 38 (88). No deaths were reported. The second outbreak was reported in Mbaki district in April 2017 accounting for 3 cases, out of which 1 was laboratory confirmed. No deaths were reported. Further investigations supported by the Ministry of Health and WHO revealed that 24 of 26 (92.3%) of close contacts had antibodies (IgG) against monkeypox, and 4 against cowpox. This suggests a high level of circulation of the virus in the region, and may explain the low number of cases recorded during these outbreaks (89).
One isolated case of monkepox was confirmed in Sierra Leone (Pujehan District) in March 2017. Thirteen close contacts were followed up and none of them have developed any febrile illness and/or skin lesions in the first 21 days since the last exposure (90).
From September 2017 through April 2018, 244 cases including 101 confirmed cases were geographically spread across 25 states and the Federal Capital Territory (FCT) of Nigeria. The confirmed cases were reported from 15 (out of 36) states (34). Six deaths were recorded (CFR 2.5). From September to December 2017, the majority of cases were male (75%) and aged 21–40 years old (median 30 years). (34, 91). The investigation established that the initial cluster of cases (two brothers, their uncle, and a neighbor) fell sick after killing and eating a captured monkey from the neighborhood, which young boys regularly played with (92). Phylogenetic analysis indicated that the closest relative of this outbreak isolates were two Nigerian strains isolated in 1971, belonging to the west African clade (44). This outbreak is the largest documented outbreak of human monkeypox in West Africa.
Sixteen cases of monkeypox, including 2 confirmed cases were reported in Liberia between November and December 2017, after more than 40 years from the last (and the first) reported occurrence. The cases were reported from Grand Cape Mount (4), Rivercress (11), and Maryland (1). Two deaths were recorded (CFR 12,5%) (93).
Between week 1 and 24 of 2018, there have been 2845 suspected cases of monkeypox in 14 provinces of the DRC, including 36 deaths (CFR 1.3%). Of the suspected cases, 34 have been confirmed samples (34). Sankuru Province has had an exceptionally high number of cases between week 1 and 14 of this year (106 cases) compared to the same time period last year (44 cases) (94).
Between 17 March and 24 April 2018, 20 cases of monkeypox were reported in CAR, including 9 cases confirmed by the laboratory (6 cases from Ippy, 3 cases from Bangassou).No deaths were recorded (34).
A total of 16 monkeypox cases have been reported in Cameroon between 30 April and 30 May 2018, including 1 confirmed case and no deaths. The cases were recorded in Njikwa Health district (7, including 1 confirmed), Akwaya Health District (6), Biyem-Assi health district (1), Bertoua Health District (1), and Fotokol Health District (1) (34).
Discussion
Monkeypox has already occurred in 10 African countries and is known to be endemic in the DRC. It has once crossed the borders of the African continent when it was imported into the USA in 2003, before which it was assumed that the disease was geographically limited. The summary of recorded cases above demonstrates an increase in the incidence of monkeypox cases in recent years, together with a broader geographical occurrence. However, the data collected is often incomplete and unconfirmed which hampers realistic estimations of prevalence and incidence of monkeypox over time. Nevertheless, the active surveillance conducted by Rimoin et al. between 2005 and 2007 concluded that there was a 20-fold increase in monkeypox incidence compared to the historic data between 1981 and 1986 (WHO active surveillance) (24). Also other official reports (e.g., DRC's passive surveillance program 2010-2016 data, see above) and unofficial source data (Table 2) underline the emerging character of the disease. Four explanations, possibly occurring simultaneously, were raised for the monkeypox incidence increase (24):
(1) The cessation of the smallpox vaccination in 1980 and the consequent drop of immunity against orthopoxviruses. Eradication of smallpox and waning immunity against after vaccine cessation created an immunologic niche for monkeypox. In 2010, only 24.5% of the DRC population had evidence of a smallpox vaccination scar. The influence of vaccination cessation is reflected in the age pattern of incidence (24, 103). After 1980, more individuals are susceptible to MPXV infection every year. Similar causality was shown for measles (104) and yellow fever (105) when a decreased vaccination coverage led to increased incidence.
(2) Higher or more frequent exposure to animal reservoir species. Significant anthropogenic and demographic changes have occurred in the DRC since 1980, and may have increased the exposure of the local population to reservoir species of MPXV. Logging of the rain forest increases the opportunities of human exposure to displaced animals, thus for zoonotic transmission of MPXV. Additionally, recurrent war, civil unrest and poverty force the affected population to flee and eventually look for shelter deeper in the rain forest, and to rely more extensively on bush meat (monkeys, small rodents, etc) (24, 106). Similar conclusions were drawn from studies on Nipah virus (107) and rabies virus (108) where environmental and anthropogenic changes led to a higher chance of exposure to (infected) animals, leading to increased incidence.
(3) Increased human-to-human transmission rate. Increased prevalence in humans, particularly immunocompromised hosts, may provide more opportunity for MPXV to acquire mutations that increase its fitness in human hosts, possibly leading to increased transmissibility, virulence, and pathogenic potential. Also probabilistic arguments suggest that a zoonotic pathogen with an R0 near to one (such as monkeypox) retains a greater potential to evolve to a state of higher transmissibility as transmission chains lengthen and as the number of primary introductions increases (16, 24, 109). This assumes that the population lacks the vaccine-derived immunity, as it is the case nowadays because the smallpox vaccination was ceased (24). It needs to be studied whether the rising monkeypox incidence is a result of increased human-to-human transmission because greater circulation among humans opens the possibility of geographic spread by travelers (24). To demonstrate, a novel H1N1 influenza virus [A(H1N1)pdm09] crossed the species barrier from swine into humans in 2009 and multiple mutations during human-to-human transmissions allowed incremental changes in viral fitness, which may have contributed to the apparent increase in disease severity (110).
(4) Advancement in diagnostic capacity and health education. Development of molecular techniques (47, 111, 112) and point-of-care systems (113) in recent years made the diagnosis of monkeypox more accurate and rapid than before. Also, more attention is paid to health education of medical workers and the general public (114). Despite these improvements which could cause higher reporting and confirming of cases, modern molecular techniques are more expensive (115), while today's surveillance programs have less funding and manpower resources than the WHO active surveillance program between 1981 and 1986. That is why the few active surveillance programs conducted nowadays are likely to be conservative estimates of a true monkeypox incidence increase (24).
The majority of data we currently have come from passive surveillance which often miss a proportion of cases, leading to an underestimation of the burden of MPXV infections in humans (18, 24). Despite this, recent research papers/reports based on passive surveillance (even though limited in number) provide evidence of the frequent occurrence of human MPXV infections (18). The incidence of monkeypox clearly increased but no detailed data is available to evaluate whether other aspects, like human-to-human transmission rate, morbidity and mortality rates or patterns of transmission changed (116).
The emergence of monkeypox as a significant human pathogen is indisputably a realistic scenario. Firstly, poxviruses were shown to be capable to rapidly adapt against host defenses despite their low mutation rates (117). Secondly, multiple countries were projected to have a suitable environment for MPXV by ecological niche modeling (82) where MPXV might be circulating undetected in animal hosts. In these countries, evolutionary, ecological, or epidemiologic changes could tip the balance in favor of emergence and possibly sustained transmission (23). A good example is Ghana where MPXV circulates in animals (118) but the country never reported human cases of MPX. The importation of MPXV-infected rodents to the USA, however, did lead to a human outbreak of MPX (50).
It is clear that surveillance but also research on the ecology, epidemiology, natural history and pathogenesis of the infection has to be addressed in order to design and implement needed prevention and control measures. Additionally, specific improvements in laboratory diagnostics and infection control measures are needed to detect cases, treat patients, and prevent further spread of the virus.
Because monkeypox is a viral zoonosis, coordination of interventions between the human and animal (wildlife) health sectors is necessary, including routine sharing of information (19). Data sharing does not only imply the animal-health sector in the context of One Health, but also inter-organization sharing as well as information sharing with the wider scientific community. Timely report publishing as a form of information sharing is a moral obligation of all health professionals. Without this common source of knowledge, there is no way to verify data obtained through passive, and in lesser amounts, active surveillance programs.
In the long run, comprehensive strategies to strengthen the health systems need to be initiated. This will enhance their resilience, in addition to building a strong preparedness and response capacity, thus avoiding outbreaks of big magnitudes in the future (86).
Conclusion
It is time that we start to take action for prevention and preparedness of epidemics, especially for pathogens we have recognized as significant human threats, like monkeypox. The available data in this review demonstrate how limited and fragmented the information about monkeypox epidemiology still is, which leads to a potential underestimation of the magnitude and severity of MPX outbreaks. This should be a wakeup call to the research community for more engagement, follow-up and research on this disease. Despite being discovered in 1958 and for the first time described in a human in 1970, there are no standard guidelines for clinical management, nor therapeutics or vaccines (23). It is also an urgent call to leading public health institutions to take their responsibility to share data with health professionals and to communicate transparently to the public as soon as it becomes possible.
Monkeypox is a significant health concern for people living in endemic regions such as DRC and other African countries where circulation of the virus is confirmed, but it is also a global health security concern as demonstrated during the USA outbreak in 2003. Appropriate and effective interventions and active surveillance activities are urgently needed to prevent increased transmission efficiency or virulence (23). MPX is the most important orthopoxvirus in humans, certainly in the endemic areas and perhaps globally. Monkeypox is not a rare disease anymore, monkeypox needs more attention.
The Commie Bullshit Never Ends
What in "HELL" is going on!
NYC Reports First Suspected Monkeypox Case As WHO Convenes Emergency Meeting
by Tyler Durden
Saturday, May 21, 2022 - 04:12 AM
Update (1608ET): Officials in New York City say they are monitoring the state's first suspected case of monkeypox in a patient receiving care at Bellevue Hospital, where preliminary tests have been performed to confirm the disease, according to the Wall Street Journal.
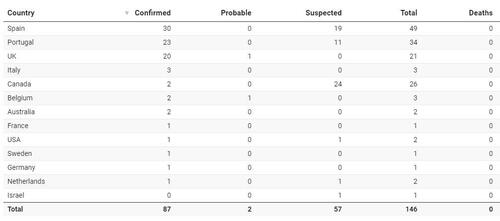
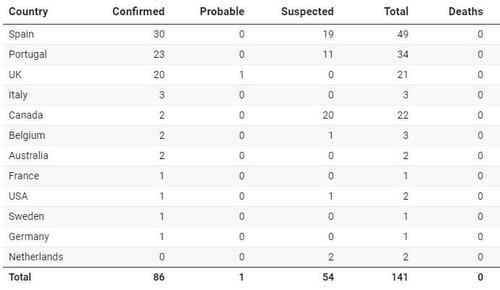
So far, 87 cases have been confirmed worldwide and 57 are under investigation, according to the World Health Organization. Earlier Friday Israel became the 13th country to report a suspected case.
The disease was also reported on Friday by Germany, Australia, France and Belgium, while two cases were confirmed in Canada.
Monkeypox causes a contagious rash similar to chickenpox in humans, and is spread through close contact. Symptoms, which usually appear within the first five days of infection, include muscle aches, chills, fever, swollen glands, exhaustion - and of course, pustules.
The mortality rate for monkeypox ranges from 1% to 15%, and is endemic in three countries; the Democratic Republic of Congo, Nigeria and the Central African Republic. The first reported case detected in the UK had traveled to Nigeria, after which they returned with a rash, according to the WHO.
Update (1055ET): The World Health Organization is convening a group of leading experts for an emergency meeting about the ongoing monkeypox outbreak, according to the Telegraph.
The meeting comes as 12 countries have reported recent cases, with the CDC confirming at least one in the United States.
"I'm sure that ultimately this will be the largest outbreak of monkeypox that we've had outside of the endemic areas in Africa," Daniel Bausch, infectious disease expert and president of the American Society of Tropical Medicine & Hygiene told Axios.
That said, Bausch doesn't think there's cause for concern just yet.
"I don't think there's a reason for panic. I don't think we're going to have tens of thousands of cases."
Prof Anne Rimoin, professor of epidemiology at the UCLA and a world renowned monkeypox expert, told the Telegraph that vaccinating close contacts of confirmed cases, also known as ring vaccination, is a good option for health officials.
She added that the public should not, at this stage, be too concerned.
"For your average person I would not be overly alarmed. If you have a rash, contact your health provider, a rash that is unusual or looks like monkeypox," she said.
"If you think you've been exposed to somebody who has monkeypox that has this kind of a rash I would I would identify yourself and talk to your healthcare provider."
So COVID was "not a major threat to the people of the US" (Fauci), Subprime is "contained" (Bernanke), and "I don't believe another financial crisis will occur in our lifetimes (Yellen)... but now we shouldn't be worried about Monkeypox...
What in the world is going on?
As Michael Snyder detailed earlier, in the past, we were told that monkeypox was not a major concern because it was so difficult to spread it from person to person.
But now monkeypox seems to be spreading like wildfire.
On May 7th, the very first case in the western world in 2022 was confirmed in the United Kingdom.
Now here we are less than two weeks later and there are now dozens of confirmed and suspected cases in twelve different countries outside of Africa.
Yesterday, I discussed the cases that have popped up in Spain, Portugal and the United States. Now there are significantly more nations that are reporting confirmed or suspected cases, and that should greatly alarm all of us.
The confirmed case in Massachusetts involves a man that had recently traveled to Canada, and so it was suspected that there were additional cases among the Canadians.
Earlier today, we learned that “thirteen probable cases are being investigated in Canada”, and the test results for those thirteen “probable cases” should be released soon.
Meanwhile, a case has been confirmed all the way up in Sweden…
‘One person in the Stockholm region has been confirmed to be infected with monkeypox,’ Sweden’s Public Health Agency said in a statement.
The infected person ‘is not seriously ill, but has been given care,’ according to the agency.
And it appears that there could be multiple cases in Italy…
Italy’s patient was holidaying in the Canary Islands and is now in isolation at the Spallanzani hospital in Rome, the hospital said.
Another two other suspected cases are being monitored, it added.
The first case of monkeypox in Australia has been confirmed in the state of Victoria from a man in his 30s who recently returned from the United Kingdom.
“There are few close contacts that have been identified, obviously the GP is one of them,” Victoria Chief Health Officer (CHO) Brett Sutton told reporters on Friday, referring to the general practitioner who referred the man for testing.
Belgium has a second case...
A case of monkeypox has been confirmed in Munich, Germany. Bavaria's Health Minister Klaus Holetschek pointed this out on Friday. The patient comes from Brazil and is already isolated in the Munich Clinic Schwabing.
A first case of infection with monkeypox was detected in France on Thursday in Île-de-France, announced this Friday the Directorate General of Health.
“As soon as his infection was suspected, this person was taken care of. In the absence of seriousness, he is isolated at his home”, specifies the ministry.
The patient is a young man of 29 with no history of travel to a country where the virus is circulating.
There may be some cases of the monkeypox virus in the Netherlands, RIVM reports Friday. Samples are currently being examined in a lab. The result of this is not yet known.
This was never supposed to happen.
Even though monkeypox is a relatively new disease, cases were always extremely rare, and a global outbreak was always considered to be extremely unlikely because it was so hard to spread monkeypox
Has something changed?
A prominent infectious disease expert at Johns Hopkins University is telling us that this virus “is spreading via physical touch”, and that it can spread “through respiratory droplets” under certain circumstances…
Dr Amesh Adalja, an infectious disease expert at Johns Hopkins University in Baltimore, Maryland, also told DailyMail.com that the virus is spreading via physical touch – and that it only spreads through respiratory droplets in the air in people that are already exhibiting symptoms.
That is extremely alarming to hear.
But before we jump to conclusions, it is important to note that we still really don’t know too much about this virus. It hasn’t been around for that long, and scientists have long warned that it could potentially mutate into a more transmissible form…
For decades, a few scientists have voiced concerns that the monkeypox virus could have become better at infecting people—ironically because we eradicated its relative, smallpox, in the late 1970s. The smallpox vaccine incidentally protected against monkeypox. And when new generations were born into a world without either smallpox or smallpox-vaccination campaigns, they grew up vulnerable to monkeypox. In the Democratic Republic of Congo, this dwindling immunity meant that monkeypox infections increased 20-fold in the three decades after smallpox vanished, as Rimoin showed in 2010. That gives the virus more chances to evolve into a more transmissible pathogen in humans. To date, its R0—the average number of people who catch the disease from one infected person—has been less than 1, which means that outbreaks naturally peter out. But it could eventually evolve above that threshold, and cause more protracted epidemics, as Bergstrom simulated in 2003. “We saw monkeypox as a ticking time bomb,” he told me.
Hopefully those that are investigating this new outbreak will soon be able to tell us whether the virus has mutated or not.
Meanwhile, authorities are claiming that it seems to be particularly spreading among men that have sex with other men. The following comes from CNN…
Both in the United Kingdom and Canada, health authorities have noted that many of the monkeypox cases were identified in men who have sex with men — but the virus is not typically described as a sexually transmitted infection and investigations into these recent cases continue.
If this new outbreak continues to grow, it will only be a matter of time before people start clamoring for vaccines. Health officials say that the existing smallpox vaccine should offer at least some protection against monkeypox, and they are already considering giving it to certain groups…
CDC officials are evaluating whether smallpox vaccine should be offered to healthcare workers treating monkeypox patients and other people who may be at “high risk” for exposure to monkeypox, McQuiston said.
“It’s definitely something that we’re discussing and evaluating, whether offering smallpox vaccine makes sense in the current setting,” she said.
“We’ll be closer to making recommendations for that in the next day or so.”
And it is being reported that there are enough doses of the smallpox vaccine “to vaccinate basically everyone in the U.S.”…
And as another bioterrorism precaution, stockpiles of three smallpox vaccines are large enough “to vaccinate basically everyone in the U.S.” Inglesby said. And though monkeypox patients usually get just supportive care, a possible treatment does exist and has also been stockpiled: Tecovirimat, or TPOXX, was developed to treat smallpox but would likely work for monkeypox too.
Hopefully we never get to a point where officials feel like a full-blown vaccination campaign is needed. After what we have been through with COVID, nobody wants to see that...
Is this where COMMIE BULLSHIT is headed?
Did You Know That A 2021 Report Predicted The Monkeypox Outbreak On May 15th 2022 ? Both Companies Involved In The Report Have Received Millions From The Bill & Melinda Gates Foundation.
Don't get the Poxy Monkey vaccine
![]()
Don't fuel their "Croc-pox" agenda!
Yes, thank you for sharing that. As posted above we said that
(Brinia, possible Britannia, where the welcome trust and pirbright have their dirty hands in the manufacturing of deadly "diseases, and vaccinations.)
@be1 ,
You are welcome.
Missed it.
Thank-you.
George W Bush under fire over ‘brutal’ Iraq invasion slip-up
Former president George W Bush is facing criticism after describing the invasion of Iraq — which he led as commander in chief — as “brutal” and “wholly unjustified” before correcting himself to say he meant to refer to Russia’s invasion of Ukraine.
Quote:
"The result is an absence of checks and balances in Russia, and the decision of one man to launch a wholly unjustified and brutal invasion of Iraq — I mean of Ukraine,” Mr Bush said during a speech at his presidential centre in Dallas.
He's not "under fire" for getting it wrong. He's getting grief for letting the cat out of the bag and inadvertently telling the truth.
*- no offense intended to @Cheeky-Monkey or any of the legendary barbary apes of the Rock ![]() If anything the above picture of Bush trying to look and act like a monkey is an insult to the monkeys.
If anything the above picture of Bush trying to look and act like a monkey is an insult to the monkeys.
Well deserving, though not of telling truth, but sea of lies.
Building narratives?
It's interesting that Spain just opened up to "unjabbed" Britons for summer vaccinations (MSN), but it is having a surge in "monkeypox" cases.
Spain now has the highest number of infections, outside places in Africa where the virus is endemic, with more than 50 known cases.
Cases of monkeypox in the UK have doubled in just a week after a total of 20 cases were reported.
And doctors warned that number will rise significantly as the virus spreads througfh Europe and as far as the US, Canada and Australia.
Are they creating a plausible "spreadibility" scenario to bring in the next pandemic – 1 of 10 they have planned between 2020-2030?
Is it really baffling – given what they have planned? Israel Reports Middle East's First Monkeypox Infection As Spread In West Baffles Experts
Monkeypox: Scenarios, Germ Games and Vaccines
By Rhoda Wilson on May 21, 2022
It appears that western governments and media are running with what Bill Gates foreshadowed as ‘the next pandemic’. This latest ‘zoonotic’ sensation appears to be the obscure and exotic monkeypox virus, which has already grabbed the headlines, as members of the embryonic global government confab, the G7, are already throwing hundreds of millions in public money at Big Pharma supposedly to ‘stop the spread.’ Déjà vu, anyone?
In the UK, Health Secretary Sajid Javid has announced that he is stocking up on smallpox vaccines to help guard against the impending scourge of monkeypox and the US government has ordered millions of doses of a vaccine that protects against monkeypox. Additionally, the World Health Organisation (“WHO”) is going to convene an emergency meeting this week on how to ‘stop the spread.’
Read more: Biden Orders Millions of Monkeypox Vaccines After One Alleged ‘Infection’, 21st Century Wire
March 2021 Monkeypox Simulation
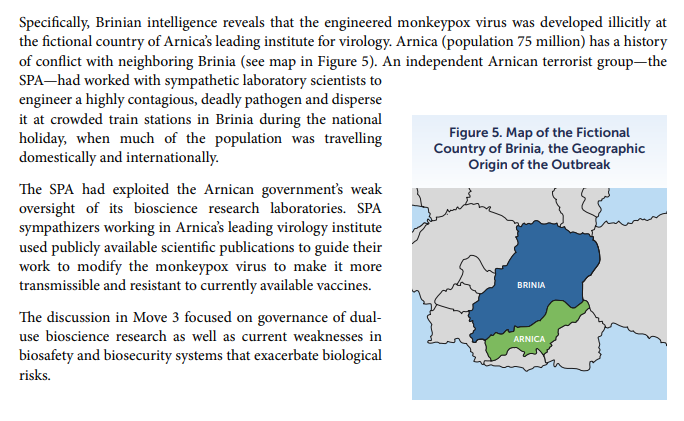
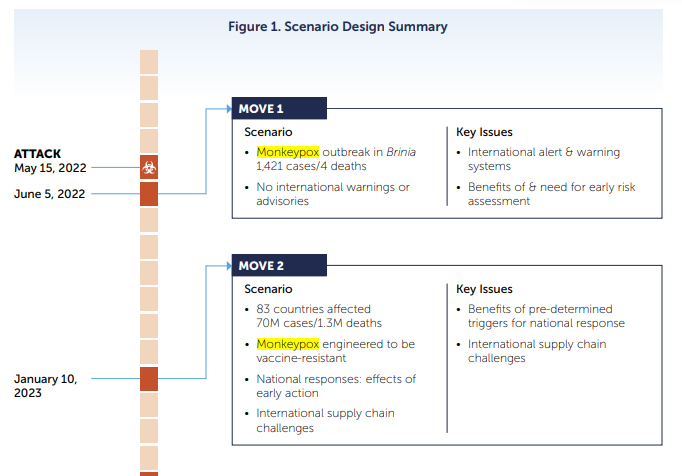
In March 2021, the Nuclear Threat Initiative (“NTI”) partnered with the Munich Security Conference to simulate “a deadly, global pandemic involving an unusual strain of monkeypox virus that emerged in the fictional nation of Brinia and spread globally over 18 months.”
NTI Paper: Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats, November 2021
“Later in the exercise, the scenario reveals that the initial outbreak was caused by a terrorist attack using a pathogen engineered in a laboratory with inadequate biosafety and biosecurity provisions and weak oversight. The exercise scenario concludes with more than three billion cases and 270 million fatalities globally.”

NTI Paper: Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats, November 2021, pg. 15
The scenario begins with an “attack” on 5 June 2022: a monkeypox outbreak with 1,421 cases and four deaths.
“Because monkeypox is not naturally found in Brinia, local and international experts consider this outbreak to be unusual. The Brinian government welcomes international outbreak investigations and requests medical support from the WHO. Genome sequencing of monkeypox patient samples reveals that the strain in Brinia contains mutations that make it resistant to existing vaccines.”
By 10 January 2023, 83 countries are affected with 1,3 million deaths and it is revealed that the monkeypox has been engineered to be vaccine-resistant.
“With no known effective therapies or vaccines, countries have had to rely principally on non-pharmaceutical interventions (NPIs) to mitigate the impacts of the pandemic.
“Highlighting significantly different national outcomes in managing the pandemic, some governments, including the fictional Republic of Dranma, promptly adopted aggressive measures to slow virus transmission by shutting down mass gatherings, imposing social-distancing measures, and implementing mask mandates. These countries have also established large-scale testing and contact-tracing operations and scaled-up their health care systems to support anticipated growing case numbers.
“By contrast, the scenario depicts another group of countries, including fictional Cardus, that have prioritised keeping their economies open, undertaking little-to-no NPIs, and downplaying the virus and its potential impacts. These countries have experienced much worse outcomes in terms of illness and mortality than those that responded early and energetically.
“Dranma experienced far fewer cases and fatalities than Cardus.”

NTI Paper: Strengthening Global Systems to Prevent and Respond to High-Consequence Biological Threats,...
Did You Know That A 2021 Report Predicted The Monkeypox Outbreak On May 15th 2022 ? Both Companies Involved In The Report Have Received Millions From The Bill & Melinda Gates Foundation.
In March 2021, the National Threat Initiative (NTI) partnered with the Munich Security Conference to conduct a tabletop exercise on reducing high-consequence biological threats. The report focused specifically on a Monkeypox outbreak.
This tabletop exercise can be added to a long list of other pandemic table top exercises. In a previous thread that I wrote back in November 2021 (before my twitter account was banned) I wrote a thread entitled “Who Are The Johns Hopkins Center for Health Security And Why Did They Publish A Document Called The SPARS Pandemic 2025-2028”. In that thread I spoke of 4 pandemic tabletop exercises that have taken place over the last twenty years such as Operation Dark Winter, Atlantic Storm, Clade X & most famously Event 201.
Continued at the link.